Currently, under thorough study is how traumatic brain injury can influence genetic activation. For survivors of mild to moderate traumatic brain injuries, the recovery process can look vastly different for each patient.
Just as no two fingerprints are alike, neither are injuries to the brain. Why do some patients breeze through treatments, rehabilitation therapy, and recovery faster while others struggle? A variety of answers surrounding the impact of traumatic brain injuries continue to evolve. From a scientific health viewpoint, one key factor is how our genomic print, otherwise known as our DNA, plays a role in traumatic brain injuries.
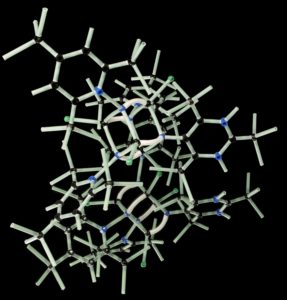 The studies of age, gender, health history, and genetics are a rising influence towards effective treatment strategies for traumatic brain injuries. In 2007, the British Journal of Anaesthesia discussed the importance of understanding patient genetic factors after traumatic brain injury. They quote, “understanding how polymorphic variants affect disease development and outcome after brain injury of any aetiology offers a number of potential benefits.” Important inflammatory markers and their associated gene pathways could provide essential information on the patient’s current or future health problems after a TBI. Medical professionals can evaluate a more comprehensive view into the patients’ health by offering the potential to restore portions of their current health condition and uncover opportunities to avert further health decline.
The studies of age, gender, health history, and genetics are a rising influence towards effective treatment strategies for traumatic brain injuries. In 2007, the British Journal of Anaesthesia discussed the importance of understanding patient genetic factors after traumatic brain injury. They quote, “understanding how polymorphic variants affect disease development and outcome after brain injury of any aetiology offers a number of potential benefits.” Important inflammatory markers and their associated gene pathways could provide essential information on the patient’s current or future health problems after a TBI. Medical professionals can evaluate a more comprehensive view into the patients’ health by offering the potential to restore portions of their current health condition and uncover opportunities to avert further health decline.
Finding the source of inflammation
After suffering from a car wreck, one patient’s health began to decline months after her injuries. She started experiencing unexplained fatigue, mood swings, nausea, dizziness, insomnia, brain fog, and severe food sensitivities that followed her every hour. She eventually became unable to keep up with her daily work, personal responsibilities, and daunting physical rehabilitation schedule. Something had to give. Upon meeting with a functional nurse practitioner, she soon learned that over-activation of a few common genetic SNPs, along with brain inflammation, gut microbiome imbalance, and neuroendocrine problems (NED) associated with a mild traumatic brain injury, were a few of the root causes for her significant health decline. Proper testing showed an elevated level of ammonia potentially triggered by a genetic over-activation of the CBS gene after her brain injury. The genetic over-activation was one of four genetic polymorphisms leading to her inability to tolerate certain foods, prescribed supplements, and common ingredients found in over-the-counter home therapeutics. The toxic combination was adding fuel to severe inflammation from her undiagnosed traumatic brain injury.
The nurse practitioner trained in functional health had extensive knowledge of epigenetics and various health conditions associated with traumatic brain injuries. The nurse spent the time needed to understand the patient’s lifestyle, symptoms, and recent head injury history. All components helped clear the path for a targeted genomic protocol. The nurse included a multi-layered plan to quickly lower the patients’ ammonia levels, restore endocrine health, hormone imbalance, micro-nutrients, and reduce inflammation. Within seven to nine months, the patient’s overall health dramatically improved. Knowing our genetic profile may sound a bit unsettling at first; however, our genes do not have to be our destiny. Due to the brain and body’s inflammatory and autoimmune response from a traumatic brain injury, something as simple as looking into our genes could help doctors improve the long-term recovery outcomes for some traumatic brain injury patients.
Understanding the benefits of whole-body healing through epigenetic therapies, nutritional guidance, and environmental influences after a TBI offers opportunities to successfully treat the root cause of chronic illnesses after a traumatic brain injury, another road toward victory for patients worldwide.
Leave A Comment
You must be logged in to post a comment.